
The rapid development of three-dimensional (3D) technology in recent years has made their integration with surgery feasible. This article introduce the application of 3D reconstruction and printing technology in personalized management of complex spinal deformities, aiming to optimize clinical decisions and elucidate the efficacy and safety of this technology.

In recent years, sports and health issues have gradually started affecting human well-being. With the advent of an aging population, skeletal health has become a significant factor influencing patients' quality of life. However, as the era of precision medicine unfolds, the high demands for efficacy have led treating physicians to seek advanced technological assistance for improved surgical outcomes. Spinal deformity diseases, with their diverse and highly individualized characteristics, impose substantial demands on orthopaedic surgeons' diagnostic and therapeutic skills. Due to the complexity of severe rigid spinal deformities, procedures such as screw insertion, osteotomy, distraction, and decompression significantly increase the risk of intraoperative neurological complications. Reports indicate that postoperative neurologic complications in complex spinal correction surgeries can reach as high as 4.0%-23%. The risk of neurological complications is closely associated with preoperative deformity severity, osteotomy location, osteotomy type, and correction rate of kyphosis deformity.
Tailoring individualized and precise surgical plannings for each patient based on their clinical and radiographic features has become a routine practice for orthopaedic surgeons. As we progress into the era of "precision medicine," the pursuit of more accurate and efficient surgical treatment strategies becomes paramount. In the field of orthopaedics, particularly in deformity cases, the three-dimensional morphological abnormalities of bones in coronal, sagittal, and axial planes result in severe loss of movement function, cosmetic deformities, and can also lead to cardiorespiratory abnormalities, significantly impacting patients' quality of life. Historically, surgical plans were often formulated based on a surgeon's personal experience and literature reports, resulting in a rudimentary assessment and prognosis of postoperative outcomes for patients, lacking visibility, specificity, and effectiveness.
Several studies have reported the use of SurgiMap software for surgical simulation to predict and design osteotomy plans. While this software provides two-dimensional correction simulations based on sagittal or coronal plane X-rays, most spinal deformities are three-dimensional in nature, limiting the applicability of two-dimensional planning software.
The rapid development of three-dimensional simulation reconstruction and 3D printing technology as advanced technologies in recent years has made their integration with medicine feasible. In various medical fields, three-dimensional imaging techniques have been utilized to reconstruct various physiological and pathological structures, simulate surgical plans, and formulate surgical strategies, gradually becoming indispensable tools for physicians. With ongoing innovations in three-dimensional reconstruction and 3D printing technologies, new cases of their integration with modern medicine continue to emerge within the medical field. In the realm of orthopaedics, this technology has also seen significant advancements in recent years. For patients undergoing orthopaedic surgery, three-dimensional reconstruction based on patient imaging data is used to create visual orthopaedic models. Precise surgical plans are developed within these visualization models, enabling the formulation of personalized surgical treatment plans for enhanced surgical outcomes and efficacy.
While computed tomography (CT) reconstruction of the spine provides three-dimensional images, traditional medical imaging still has limitations in preoperative planning and intraoperative guidance. 3D printing technology based on CT scan data can provide surgeons with high-precision, anatomically accurate physical spine models. Recent studies have shown that these models not only play a crucial role in educating medical students and explaining patient conditions and surgical plans but also assist surgeons by visualizing anatomical structures and tissues, ultimately reducing surgical time.
Previous research has demonstrated that 3D printing technology contributes to improved accuracy of pedicle screw placement, reduced surgical time, decreased surgical blood loss, and lowered neurological complications. Some scholars have reported the combined use of digital technology and 3D printing for preoperative planning and pedicle osteotomy in complex spinal deformity surgeries. They constructed osteotomy guides and simulated the surgical process, proving that the 3D printing osteotomy guide system could effectively assist in preoperative osteotomy planning. However, this experiment was conducted in vitro, which limits the value of this personalized design and assisted surgery system. Therefore, the value of personalized digital planning combined with 3D printing technology in assisting osteotomy procedures for rigid complex spinal deformities still requires further exploration.
Through three-dimensional simulation reconstruction and 3D printing technology, various preoperative data, surgical plans, and postoperative effects can be visualized, enabling surgeons to more accurately assess postoperative skeletal structural conditions. Moreover, the application of relevant internal fixation and osteotomy guides created from three-dimensional simulations can significantly enhance the surgical effectiveness and safety. Presently, this technology has yet to be fully integrated. In this article, we would introduce the application of three-dimensional reconstruction and 3D printing technology in personalized surgical treatment of complex severe spinal deformities by our team, aiming to optimize clinical decisions and elucidate the clinical efficacy and safety of this technological approach.
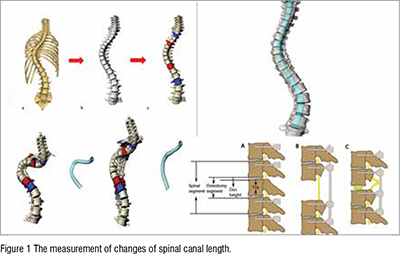
Han et al. assessed the effects of two surgical techniques, Ponte osteotomy and posterior vertebral column resection (PVCR), on spinal cord deformation in severe and rigid kyphoscoliosis patients. A 3D model of the spine was constructed for each patient, focusing on the spinal canal between T2 and L2 vertebrae. Results revealed that Ponte osteotomy elongated the spinal canal length (SCL) at the concave side by 5.4% and at the convex side by 1.3%, while PVCR shortened SCL at the concave side by 2.3% and at the convex side by 5.2%. Both techniques significantly improved Cobb angles and patient-reported outcome measures, with Ponte osteotomy primarily elongating the SCL at the concave side and PVCR causing compression at the convex side. These findings offer insights for the development of new surgical techniques that integrate the benefits of both approaches to optimally correct spinal deformities and prevent neurological complications. Also, this is the first time that the spinal canal reconstruction technique was applied in complex spinal deformity evaluation.
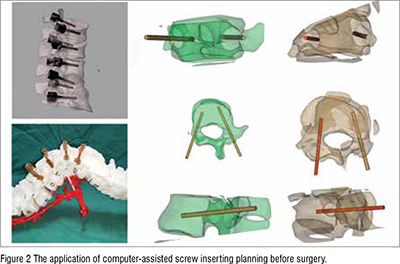
Zhang et al. conducted a prospective cohort study aiming to investigate the feasibility and effectiveness of computer-assisted screw inserting planning (CASIP) in treating severe spinal deformities. A total of 50 patients participated, with 25 allocated to the CASIP group and 25 to the Non-CASIP group. Pedicle screw accuracy, puncturing rates, estimated blood loss, surgical time, correction rate, and radiological parameters were compared between the two groups. The CASIP group demonstrated significantly higher pedicle screw accuracy (92.0 ± 5.5% vs. 82.6 ± 8.3%, P < 0.05) and lower puncturing rates (0% vs. 0-6.25%, P < 0.05) compared to the Non-CASIP group. Additionally, the CASIP group exhibited shorter surgical times (280.0 [IQR: 260.0-300.0] min vs. 310 [IQR: 267.5-390.0] min, P < 0.05). This study concluded that CASIP is feasible and enhances the accuracy of pedicle screw placement, enabling spine surgeons to create detailed preoperative personalized screw plans, resulting in improved fixation outcomes.
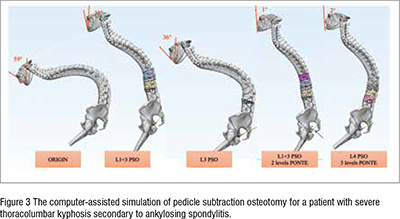
Zhang et al. assessed the reliability of computer-assisted three-dimensional surgical simulation (CA3DSS) for posterior osteotomies in thoracolumbar kyphosis secondary to ankylosing spondylitis (TLKAS) patients. Simulated osteotomies were conducted using Mimics and 3-Matic Medical software, and radiological parameters were measured in preoperative X-rays, preoperative original 3D spine (Pre-OS), simulated 3D spine (SS), and postoperative original 3D spine (Post-OS). Reliability was assessed through intraclass correlation coefficients (ICCs) and Bland-Altman analysis. The study found excellent consistency between preoperative X-rays and Pre-OS models. In SS and Post-OS models, global kyphosis, thoracic kyphosis, and lumbar lordosis exhibited excellent reliability (ICC 0.832, 0.773, and 0.896, respectively), while the main curve and sagittal vertical axis showed good reliability. Correction angles achieved by pedicle subtraction osteotomy (PSO) and posterior column osteotomies (PCO) also demonstrated good reliability. Bland-Altman analysis further supported the agreement between Cobb angle and distance measurements. The study concludes that CA3DSS is an accurate, reliable, and effective method for simulating correction surgery with posterior osteotomies in TLKAS patients.
Pan et al. performed a retrospective case-control study aiming to assess the utility of three-dimensional printing (3DP) spine models in the surgical management of severe spinal deformities. Patients with severe scoliosis or hyper-kyphosis who underwent posterior fixation and fusion surgery using 3DP spine models were compared to a control group that underwent surgeries with free-hand screw implantation. After propensity score matching, 35 patients were included in each group. The 3DP group exhibited significantly reduced operation time and blood loss compared to the control group. Moreover, the 3DP group demonstrated higher accuracy in pedicle screw placement and a lower rate of screw misplacement-related complications. Notably, a higher proportion of three-column osteotomies were performed in the 3DP group. This study emphasizes that 3DP spine models can enhance surgeons' confidence in executing complex osteotomies and improve safety and efficiency in severe spinal deformity correction surgery. The promising potential of 3D printing technology in spinal deformity surgery is highlighted.

Liang et al. performed a study to compare the accuracy of pedicle screw placement and surgical outcomes between the 3D-printed (3DP) guide template technique and the freehand technique in spinal deformity surgery. Through a systematic literature search, seven studies involving 87 patients with 1384 pedicle screws placed using 3DP guide templates and 88 patients with 1392 pedicle screws placed using the freehand technique were included in the meta-analysis. The results indicated that the 3DP template technique exhibited significantly higher accuracy for placing pedicle screws, with increased rates of excellently and qualifiedly placed screws, and decreased rates of poorly placed screws. Additionally, the 3DP template group demonstrated reduced mean placement time per screw, total screw placement time, and blood loss compared to the freehand group. Notably, there were no significant differences in operation time and main curve correction rate between the two techniques. In conclusion, this study highlights the potential of the 3DP guide template as a promising tool to enhance pedicle screw placement accuracy in spinal deformity surgery, warranting further adoption and exploration.

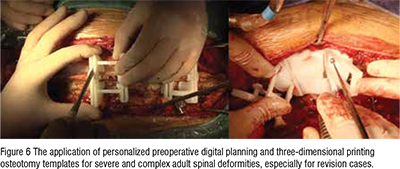
Ding et al. demonstrated the clinical utility of personalized preoperative digital planning and three-dimensional printing (3DP) guide templates for the treatment of severe and complex adult spinal deformities. The procedure included osteotomy. Various perioperative and radiological parameters were collected and analysed retrospectively. The technique achieved successful outcomes, with correction of main cobb angle and kyphosis and a high ratio of osteotomy execution to simulation (97.02%). Notably, three pedicle subtraction osteotomies (PSOs) and five vertebral column resection (VCR) osteotomies were conducted with the assistance of the guidance templates. The study concludes that this approach is effective, safe, and easily applicable, allowing for precise preoperative osteotomy simulation and reducing surgical risks and complexities associated with high-level osteotomy in severe adult rigid deformities.
Precision medicine's emergence has prompted orthopaedic surgeons to seek advanced technological support for improved surgical outcomes. Among the complex challenges posed by spinal deformity diseases, the demand for personalized and precise surgical planning has led to the integration of three-dimensional morphological assessments and 3D printing technology. These innovations enable the creation of patient-specific orthopaedic models, serving as the foundation for meticulous surgical plans tailored to individual needs. The studies presented in this collection highlight the transformative potential of advanced technologies in spinal deformity treatment. From investigating the impact of osteotomy techniques on spinal cord deformation to enhancing pedicle screw accuracy through computer-assisted planning and leveraging three-dimensional surgical simulation for complex cases, these techniques underscore the potential of computer technology in optimizing surgical interventions. Moreover, the application of 3D-printed spine models and guide templates demonstrates tangible improvements in surgical efficiency, accuracy, and safety. As technology continues to reshape the field of orthopaedics, these advancements hold promise for enhancing patient outcomes and redefining the standards of care in spinal deformity treatment.